World Chronic Obstructive Pulmonary Disease Day | Under the epidemic, we should care for life and health

Since 2002, the third Wednesday of November of each year has been established as World Chronic Obstructive Pulmonary Disease Day, through the active initiative of multinational respiratory disease experts. Each year, the Global Initiative for Chronic Obstructive Lung Disease (GOLD) selects a theme to coordinate global resources to prepare for various activities in order to improve the understanding of chronic obstructive pulmonary disease (COPD).
World Chronic Obstructive Pulmonary Disease Day
Chronic obstructive pulmonary disease (COPD) is a common, preventable, and treatable disease characterized by persistent respiratory symptoms and airflow limitation, usually due to abnormalities of the airways and/or alveoli caused by significant exposure to toxic particles or gases. The characteristic pathological changes of chronic obstructive pulmonary disease are manifested in the airways, pulmonary parenchyma and pulmonary vessels, chronic inflammation with specific inflammatory cell increase in different parts of the lung tissue, and structural changes after repeated injury and repair.
The morbidity, morbidity, and mortality of COPD vary from country to country, and even among different populations within the same country. Chronic obstructive pulmonary disease is the result of long-term cumulative exposure to toxic gases and particles, as well as complex interactions between various patient host factors including genes, airway hyperresponsiveness, and pulmonary dysplasia at an early age.
The morbidity, morbidity, and mortality of COPD vary from country to country, and even among different populations within the same country. Chronic obstructive pulmonary disease is the result of long-term cumulative exposure to toxic gases and particles, as well as complex interactions between various patient host factors including genes, airway hyperresponsiveness, and pulmonary dysplasia at an early age.
Diagnosis
The clinical diagnosis of chronic obstructive pulmonary disease should be considered in any patient with a history of dyspnea, chronic cough or sputum production, and/or exposure to risk factors. Pulmonary function test is a necessary condition for the diagnosis of chronic obstructive pulmonary disease. Pulmonary function should determine forced vital capacity (FVC) and forced expiratory volume in the first second (FEV1), and calculate their ratio (FEV1/FVC). The presence of persistent airflow limitation can be determined if the post-bronchodilator FEV1/FVC is < 70%. Chronic obstructive pulmonary disease can be diagnosed if there are corresponding symptoms and significant exposure to risk factors.
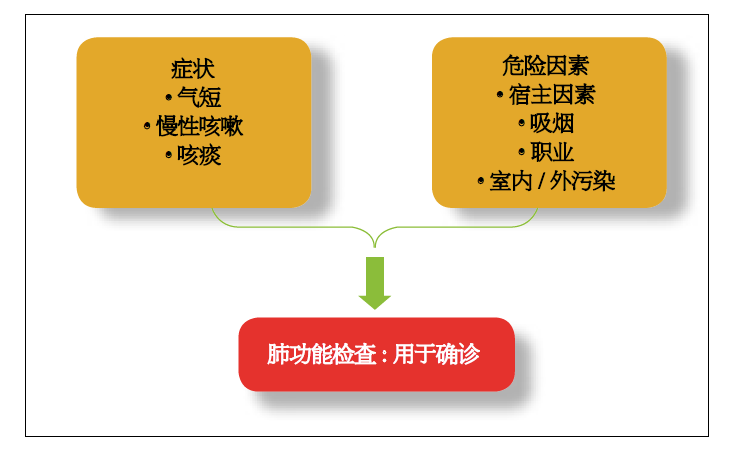
Table: Diagnostic Pathways for Chronic Obstructive Pulmonary Disease
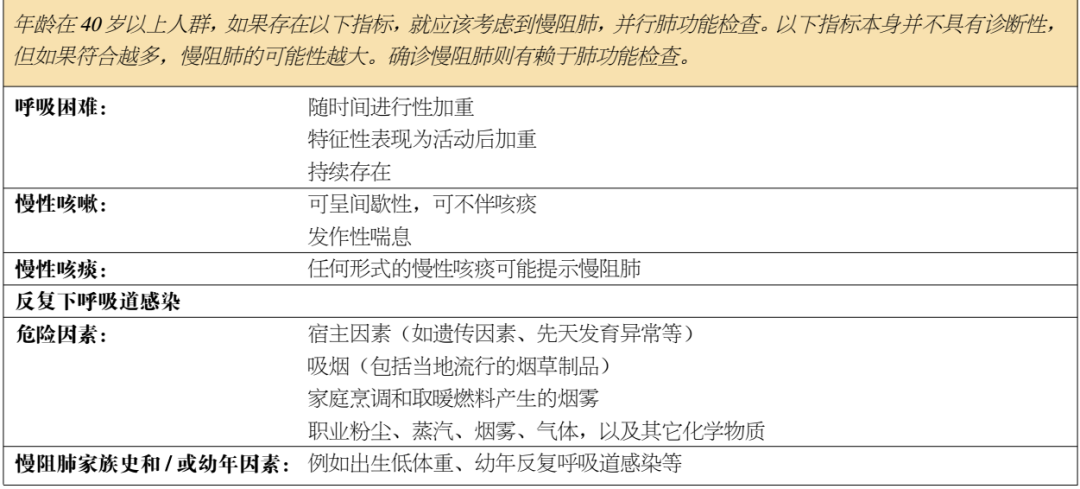
Table: Key Points to Consider for Diagnosis of Chronic Obstructive Pulmonary Disease
Assessment
The purpose of chronic obstructive pulmonary disease (COPD) assessment is to determine the level of airway limitation and its impact on the patient's health status, as well as the risk of future adverse events (such as acute exacerbation, hospitalization or death), so as to finally guide the treatment. Patients with chronic obstructive pulmonary disease are often associated with chronic diseases such as cardiovascular disease, skeletal muscle dysfunction, metabolic syndrome, osteoporosis, depression, and lung cancer. Given that these comorbid conditions are independent risk factors affecting patients' hospitalization and death. Therefore, patients with chronic obstructive pulmonary disease should be actively sought to assess comorbid diseases and give the correct treatment.
In order to achieve these goals, the evaluation of chronic obstructive pulmonary disease should consider the following aspects:
· Pulmonary dysfunction and its severity
· Nature and degree of the patient's current symptoms
· History of exacerbations and future risks
· Presence of concomitant diseases
Medication
Pharmacological treatment can relieve chronic obstructive pulmonary disease symptoms, reduce the frequency and severity of exacerbations, and improve health status and exercise tolerance. So far, in clinical studies, no drug for chronic obstructive pulmonary disease can delay the long-term decline in lung function. The choice of each drug depends on accessibility, medical costs, and the trade-off of clinical effectiveness and side effects. Each treatment method needs to be individualized because symptom severity, the condition of airflow limitation, and the degree of exacerbations vary between patients.
There are a variety of drugs for the treatment of chronic obstructive pulmonary disease, such as bronchodilators, expectorants and glucocorticoids. Bronchodilators are the most widely used drugs in patients with chronic obstructive pulmonary disease, and their therapeutic effects will be emphasized below.
There are a variety of drugs for the treatment of chronic obstructive pulmonary disease, such as bronchodilators, expectorants and glucocorticoids. Bronchodilators are the most widely used drugs in patients with chronic obstructive pulmonary disease, and their therapeutic effects will be emphasized below.
4.1 Bronchodilators
Bronchodilators can increase FEV1 or improve other pulmonary function parameters, and the principle of improving expiratory airflow is to cause airway dilatation by changing the tension of airway smooth muscle, rather than changing the elastic resistance of the lung. Therefore, such drugs reduce dynamic hyperinflation and improve exercise endurance both at rest and in the active state.
Bronchodilators can increase FEV1 or improve other pulmonary function parameters, and the principle of improving expiratory airflow is to cause airway dilatation by changing the tension of airway smooth muscle, rather than changing the elastic resistance of the lung. Therefore, such drugs reduce dynamic hyperinflation and improve exercise endurance both at rest and in the active state.
4.1.1 Beta2-agonists
The action of β2 receptor agonists is to relax airway smooth muscle by activating β2 adrenoceptors, which in turn increase cAMP and functionally antagonize bronchoconstriction. Β2 receptor agonists are divided into short-acting (SABA) and long-acting (LABA). The bronchodilator effect of short-acting β2 agonists is generally maintained for 4 to 6 hours. Regular and as-needed use of short-acting beta-agonists can increase FEV1 and improve symptoms. For patients with chronic obstructive pulmonary disease, a single dose, on-demand use of levosalbutamol does not have an advantage over a routinely used bronchodilator. LABAs showed a sustained effect of 12 hours or more and did not preclude the additional benefit of on-demand SABA therapy.
Among LABAs, formoterol and salmeterol twice daily significantly improved FEV1, lung volume, dyspnoea symptoms and health status, and reduced the frequency of exacerbations and hospitalisations, but had no effect on mortality or the rate of decline in lung function. Indacaterol can improve dyspnea, health status, and frequency of exacerbations when used once daily. Some patients experienced cough after inhalation of indacaterol. In addition, olodaterol and vilanterol are also once-daily LABAs that can improve lung function and improve symptoms.
4.1.2 Anticholinergics
Anticholinergics block the bronchoconstrictive effect of the acetylcholine muscarinic receptor M3, which is expressed on airway smooth muscle. Short-acting anticholinergics (SAMAs) such as isopropyl and oxitropium also block the inhibitory neuronal receptor M2, which can potentially cause vagally induced bronchoconstriction. Long-acting anticholinergics (LAMAs) such as thiotropium bromide, aclidinium bromide, glycopyrrolate and umeclidinium bromide bind to the M3 muscarinic receptor in a long-lasting manner, rapidly dissociating from the M2 muscarinic receptor, thereby prolonging the bronchodilator effect.
4.1.3 Methylxanthines
The exact efficacy of xanthine derivatives remains controversial. They are nonselective phosphodiesterase inhibitors and have been found to have many nonbronchodilator effects. Theophylline is the most widely used methylxanthine and is metabolized by cytochrome P450 mixed-function oxidases. Evidence suggests that theophylline has a moderate bronchodilator effect compared with placebo in stable chronic obstructive pulmonary disease. Salmeterol combined with theophylline was more effective than salmeterol in improving FEV1 and dyspnea symptoms. Evidence that low-dose theophylline can reduce the onset of exacerbations is still limited and conflicting.
A major problem with xanthine derivatives is that they have a narrow therapeutic window, have an effect dose close to the toxic dose, and are highly susceptible to the risk of overdose. Side effects include atrial and cardiac arrhythmias (which can be fatal) and convulsions (regardless of a history of seizures). Other side effects include headache, insomnia, nausea, and heartburn, which can occur when serum theophylline concentrations are still within the therapeutic dose range.
4.2. Combined bronchodilator therapy
The combination of bronchodilators with different mechanisms of action and duration of action can increase the degree of bronchodilation and reduce the risk of side effects compared with increasing the dose of a single bronchodilator. For example, the combination of SABAs and SAMAs can improve FEV1 and symptoms better than any drug. Formoterol and thiotropium bromide had a greater effect on FEV1 in different inhalers than either drug alone. A number of LABAs and LAMAs have been combined with a single inhaler to improve lung function compared with placebo, and this improvement is greater than with long-acting bronchodilators alone.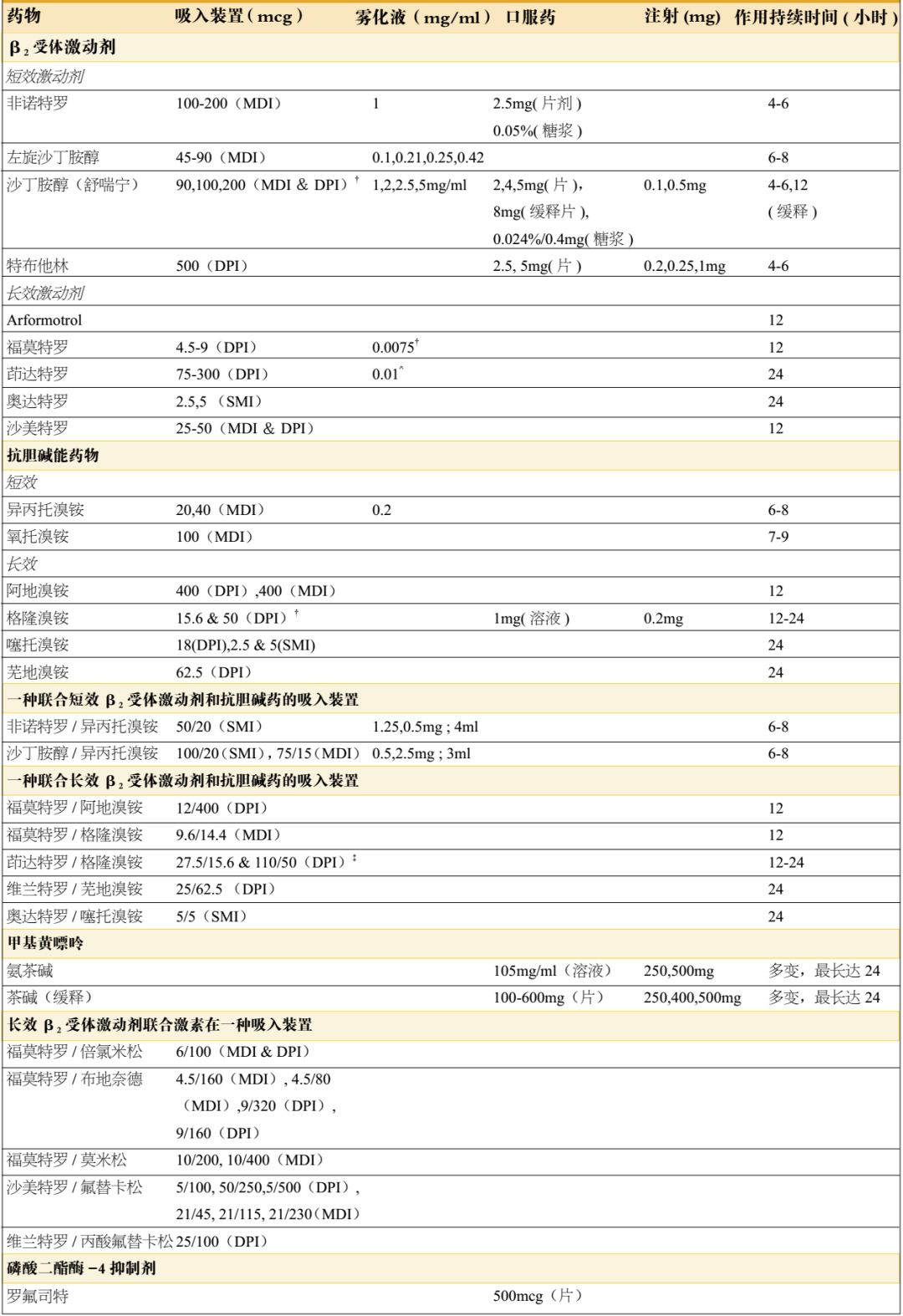
Table: Commonly used maintenance drugs for chronic obstructive pulmonary disease
The combination of bronchodilators with different mechanisms of action and duration of action can increase the degree of bronchodilation and reduce the risk of side effects compared with increasing the dose of a single bronchodilator. For example, the combination of SABAs and SAMAs can improve FEV1 and symptoms better than any drug. Formoterol and thiotropium bromide had a greater effect on FEV1 in different inhalers than either drug alone. A number of LABAs and LAMAs have been combined with a single inhaler to improve lung function compared with placebo, and this improvement is greater than with long-acting bronchodilators alone.
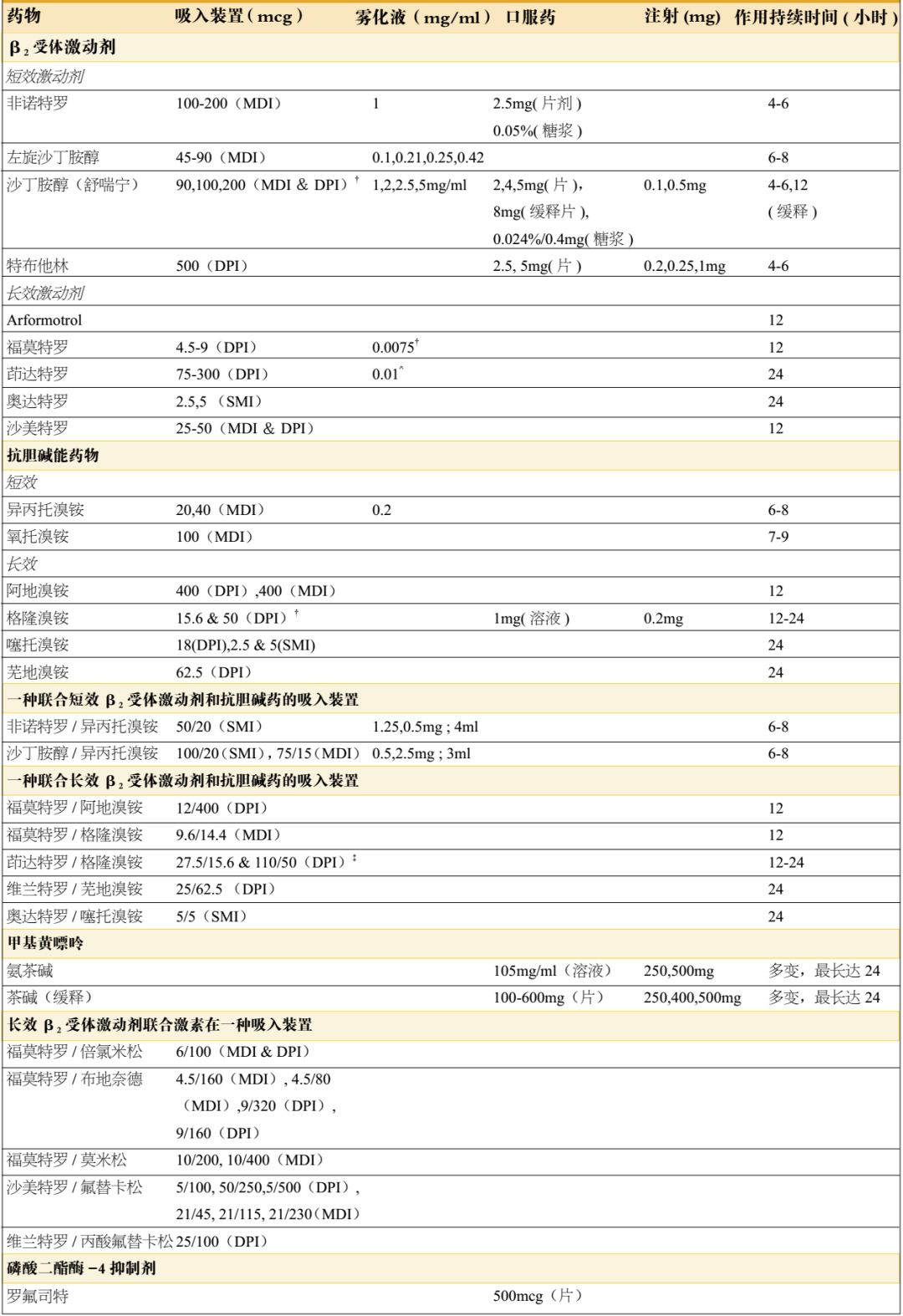
Table: Commonly used maintenance drugs for chronic obstructive pulmonary disease
Use of the suction device
Since the drugs used by most patients with chronic obstructive pulmonary disease are inhaled, the correct operation method is essential for exerting efficacy. The inhalation devices include nebulizers, metered-dose inhalers (MDIs) without storage tank, soft mist inhalation devices, respiratory-driven devices such as respiratory-driven MDIs (BAIs), and single-dose and multi-dose dry powder inhalers (DPIs). Observational studies have found a significant relationship between inappropriate use of inhaler devices and symptom control in chronic obstructive pulmonary disease. The determinants of inappropriate use of inhalation methods in patients with asthma and chronic obstructive pulmonary disease include: old age, use of multiple devices, and previous lack of education on inhalation methods, so education and training on the use of inhalation devices should be very emphasized when inhalation therapy is given.
The key points about inhaled drugs are as follows:
The choice of inhalation device needs to be individualized and depends on accessibility, price, prescriber, and more importantly the patient's capabilities and preferences.
It is important that patients be instructed and given appropriate inhalation techniques to prescribe the device to ensure they are using it correctly, and at each visit to re-check that they are using it correctly.
Inhalation techniques and treatment compliance should be assessed before determining that the current treatment regimen requires adjustment.
The World Health Organization sets World COPD Day in order to help people improve their understanding of COPD and improve the current status of underdiagnosis and poor treatment of COPD. As a part of the pharmaceutical industry, we should bear this responsibility. As a CRO service provider with both depth and temperature, Yidu Zhengkang assisted a number of pharmaceutical companies to carry out clinical research and registration services of respiratory drugs such as chronic obstructive pulmonary disease, and successfully assisted China's first original (First-in-class) stem cell new drug IND in 2020. This product is an autologous reinfusion preparation of REGEND001 cells owned by Xianhe Medical Co., Ltd. On July 15, 2020, it was approved by CFDA for drug clinical trials (Approval Letter No.: CXSL1900019) for the treatment of early and middle idiopathic pulmonary fibrosis. We also hope that more pharmaceutical companies will pay attention to the field of chronic obstructive pulmonary disease and cooperate with each other to provide better medication options for patients.
REFERENCES:
2017 GOLD Global Initiative for Chronic Obstructive Pulmonary Disease: Global Strategy for the Diagnosis, Treatment and Prevention of COPD (Chinese Version)


